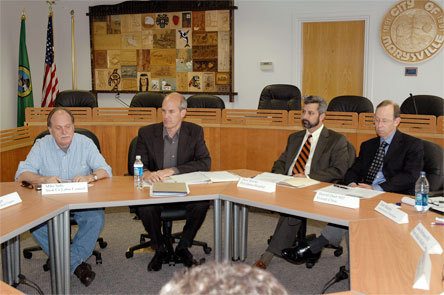
MARYSVILLE — More than a dozen representatives of local health care providers, advocates, patients, local businesses, hospitals and other groups met with U.S. Rep. Rick Larsen, July 6 in the Marysville City Council Chambers, to discuss health care reforms for Northwest Washington families and businesses.
Larsen explained that three committees in the U.S. House of Representatives are working on one draft for health care reform, and listed his priorities as allowing those who prefer their current health care providers to keep them, ensuring that health care costs are affordable, preventing discrimination based on pre-existing conditions, and eliminating geographic variances that result in some regions paying more for the same standards of care.
Mike Sells, secretary and treasurer of the Snohomish County Labor Council, relayed labor’s support for both the public option and the pay-or-play requirement, as well as their reservations about having their health care taxed.
Larry Kalb, president of Health Care For All, expressed his preference for a single-payer system, since “the holes in our safety net are getting bigger,” in part because of significant drops in sales tax revenues. While he supports “a public plan,” he’s not necessarily in favor of the public option. He urged Larsen to seek out strategies with less bureaucracy, asserting that the savings could put more money in people’s pockets, thereby stimulating the economy.
Kerri Lenderman, executive director of the Whatcom Alliance For Healthcare Access, has seen an increase in traffic as more employers have dropped health care coverage and more workers are left unsure about what levels of health care, if any, they might qualify for. She described a number of families as on the brink of “financial disaster” as a result of health care-related expenses. At the same time, she acknowledged that universal health care is ideal, but “I don’t see it happening.” She nonetheless would like to see a system that everyone pays into.
Alex Kosmides, deputy director for the Northwest Workforce Council, emphasized the importance of supporting career movement and diversity for health care providers. He advocated rewards for health care workers who use their own education and experiences to teach and train others in those roles, and identified shifts to preventive home care and home health interventions as means of utilizing nursing assistants more effectively. Decrying “the rising cost of transparency,” he asserted that employees shouldn’t need to be accountants in order to understand or obtain information from insurance companies.
Alan Friedlob, assistant director of the Critical Juncture Institute at Western Washington University, warned against potential lobbying diversions in the health care debate, as well as the potential problems of selling conservative citizens on a public plan. Although Friedlob supports such a plan himself, and agreed with Larsen’s earlier assessment that “if you’re waiting for the health care reform train to move, you’re too late, because it’s already moving,” Friedlob pointed out that “not everyone is in the train.”
Ingrid MacDonald, advocacy director for AARP Washington, noted the medical needs of the aging Baby Boomer population. Although she stated that people should not be forced to pay more than 10 percent of their incomes on health care, she cited the number of people on Medicare who are paying as much as 30 percent of their incomes on health care. She identified the high costs of prescription drugs as a problem, and suggested alternatives such as generic versions of biologics.
Arlington resident Tom Monroe, statewide volunteer coordinator of the AARP Driver Safety Program, added that premiums have become so high that some people can no longer afford to purchase health insurance, which can put them “hundreds of thousands of dollars in the hole” when they require care.
Jack McRae, senior vice president of government affairs for Premera Blue Cross, voiced his support for 80 percent of the House tri-committee health reform draft, notably its language on tort reform, but he worries that a public option has the potential to lead toward a single-payer system.
Dave Brooks, CEO of Providence Regional Medical Center in Everett, advocated on behalf of comprehensive reform, warning that, if only a few aspects are improved, it will be “like squeezing one end of a balloon.” He reiterated the need for affordability and accessibility, especially for poor and otherwise vulnerable patients, since Providence serves as a safety net for many such charity cases.
Deb Murphy, CEO of Aging Services of Washington, echoed the support voiced by Brooks and McRae for “much of this bill,” and identified the need to fix the broken Medicare system, pointing out its tendency to overpay or underpay. She regards the current stop payment tool, for keeping health care staff in line, as unduly punitive and sees a difficulty in retaining qualified staff when they receive less payment for their services. She suggested a repeal on therapy caps, by promoting therapy as “effective at keeping people in their homes.”
Laura Hoffmann, director of nursing services at the Warm Beach Health Care Center, described the evolution of nursing homes “from family environments into sterile ones,” and asserted that the suggested choice between caring for children or caring for seniors is a false dichotomy, especially since “everyone will be senior citizens eventually.”
Dr. Harold Dash, board president of the Everett Clinic, emphasized quality, access and equity, as well as value over volume in clinic reform, rather than simply paying by the numbers of times that patients are seen. He noted that preventive care can be administered via low-tech methods such as follow-up visits, and having hospice nurses help take care of patients.
Steve Kofahl, president of the American Federation of Government Employees Councils 215, 220 and 224, is also a member of Health Care For America NOW! who sees people falling through the cracks. He believes that Medicare is most in need of reform, since “a lot of people just miss the eligibility threshold,” and he insisted that the public option must be robust in order to drive costs down. He cited the amount of money spent by the health care industry on advertising, lobbying, administration and executive pay, and called for a discussion of a single-payer system, since other countries have it.
Everett ER physician Dr. Cynthia Markus, president of the Washington State Medical Association, supports a public plan but is concerned about the details. She expressed a desire to preserve the private insurance market, but also suggested that individual states be allowed to experiment with methods of providing health care, so that “we can learn from local mistakes before they go nationwide.” She gave the draft a lot of points for its tort reform language.
Larsen concluded by promising that, by the end of July, Congress will have passed some version of health care reform.